- Hotline: 852+ 2891 9689
- Whatsapp: 852+ 9146 8426
- [email protected]
- 6/F 29 Austin Road, Tsimshatsui, Kowloon, Hong Kong
A Protocol to Avoid Unnecessary Antibiotics
Home » Our Innovation – Postop Folliculitis Prevention
In most cases, no. True bacterial infections are rare. The majority of post-op folliculitis is either an inflammatory response to surgical trauma or a foreign-body reaction to hair fragments, not an infection requiring antibiotics. Misdiagnosis leads to unnecessary antibiotic use, which carries its own risks without addressing the root cause.

Post-operative folliculitis—small, inflamed bumps on the scalp—is a common but often misunderstood healing response after a hair transplant. Our clinical research, published in the ISHRS Forum, shows that most cases are inflammatory or foreign-body reactions, not true infections. Our targeted prevention protocol, including precise surgical technique and a short course of anti-inflammatory medication, has drastically reduced its incidence, eliminating the need for routine prophylactic antibiotics in most patients.


Based on our published research, we classify recipient-site folliculitis into three distinct types by cause and timing:
Traumatic Folliculitis (Early Onset: Days 1-7): An inflammatory response triggered by surgical trauma, released sebum, or buried skin fragments during graft placement. Common in patients with oily skin or seborrheic dermatitis.
Foreign-Body Folliculitis (Delayed Onset: Weeks 1-12): A reaction caused by dislodged hair fragments from transplanted follicles being perceived as foreign material by the immune system. More common with coarse hair and dense packing.
Infective Folliculitis (Variable Onset): A true bacterial infection. This is uncommon and typically only occurs with significant barrier breakdown, poor hygiene, or underlying health conditions.
Our prevention strategy is proactive and multi-layered, focusing on minimizing inflammation.
Refined Surgical Technique: Meticulous graft preparation and placement to reduce trauma and avoid burying epithelial fragments.
Targeted Pre-Op Preparation: For high-risk patients (oily skin, acne), we may recommend pre-operative anti-inflammatory medication (e.g., doxycycline) and medicated shampoo.
Post-Op Anti-Inflammatory Protocol: A key component is a short, tapering course of oral corticosteroids (e.g., Prednisolone) immediately after surgery. This significantly reduces general inflammation and has markedly decreased our folliculitis incidence.
No Routine Prophylactic Antibiotics: We do not prescribe antibiotics “just in case,” as they do not prevent inflammatory folliculitis and contribute to antibiotic resistance and patient risk.
Treatment is specific to the type diagnosed, emphasizing minimally invasive intervention first.
For Inflammatory (Traumatic) Folliculitis: Careful drainage of pustules, topical anti-inflammatory/antibiotic combinations, and continued medicated washing. Systemic antibiotics are rarely needed.
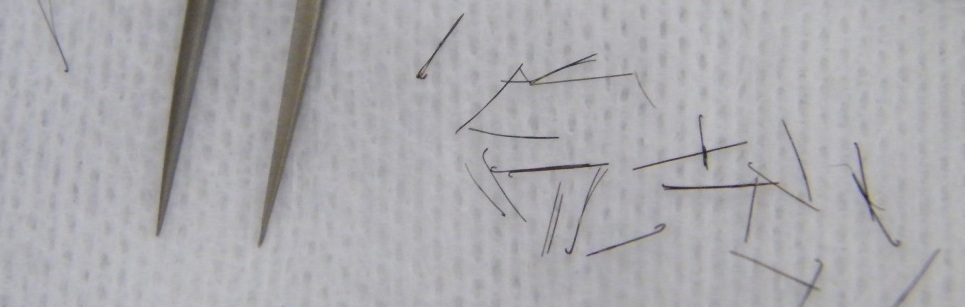
For Foreign-Body Folliculitis: The core treatment is gentle removal of the embedded hair fragment with tweezers, which provides immediate relief. Anti-inflammatory topical agents support resolution.
For True Infection: Requires culture and targeted systemic antibiotics. This is rare in our practice due to our prevention and hygiene protocols.
This distinction is central to ethical, effective care.
Avoids Patient Harm: Preventing the overuse of antibiotics spares patients potential side effects and allergic reactions.
Promotes Proper Healing: Correctly treating inflammation with anti-inflammatory measures (steroids, drainage) leads to faster, more comfortable resolution.
Upholds Medical Standards: It reflects an evidence-based, biologically accurate understanding of the healing process, moving beyond a one-size-fits-all drug prescription.
Most Folliculitis is Not an Infection: The majority of post-transplant bumps are inflammatory or foreign-body reactions, not bacterial infections.
Prevention is Protocol-Based: Our preventive strategy uses surgical precision and targeted anti-inflammatory medication (like short-course steroids) to significantly reduce occurrence.
Treatment is Cause-Specific: Effective management requires correct diagnosis—drainage and anti-inflammatories for trauma, hair fragment removal for foreign-body reactions, and antibiotics only for confirmed infection.
Routine Antibiotics Are Not the Answer: Prescribing prophylactic antibiotics for folliculitis is often ineffective and unnecessary, aligning with our commitment to minimizing patient risk and antibiotic resistance.
A proper surgical plan includes managing the healing process. Discuss our folliculitis prevention protocol and our philosophy of minimizing unnecessary medication during your consultation. We will explain how our approach is designed to ensure not only great results but also a smooth, comfortable recovery.

Images & Information shown are for reference only
Information on this website is provided for general educational purposes only and does not constitute personalized medical advice. It is not intended to promote our service or imply superiority over another.
Individual results in hair restoration vary significantly and no outcome can be guaranteed. The before-and-after images shown represent possible results — not promises. We recommend seeking independent medical advice to discuss your options … Read More
Paragraph

Pre-Consultation Review
If you want to get a personalized answer from our medical team, you can reach us using this form here. We will cantact you as soon as possible.
Our practice adheres to guidelines established by leading international organizations in Hair Restoration.
International Society of Hair Restoration Surgery is the leading global medical association that establishes international practice standards and patient safety protocols.

The American Board of Hair restoration Surgery represents the highest standard. To maintain rigorous certification requirements the physician must demonstrate surgical expertise.
Worls FUE InstituteI serves as the premier educational body focused exclusively on Follicular Unit Extraction methodology. The institute ensures consistent application of safe FUE.